Many healthcare providers are overwhelmed by administrative tasks. These duties can make it challenging for you to keep your practice afloat. Medical billing companies have emerged as invaluable allies for healthcare providers. If you work with them, they’ll increase the flow of your revenue and let you focus on what you do best—providing exceptional patient care.
So, if you’re worried about how to streamline your practice’s financial operations and enhance the quality of care you provide, you’re in the right place. In the following sections, you’ll learn about seven crucial services that can increase your medical billing business income and the transformative impact they can have on your practice.
I would like you to act as my writing assistant. I’m going to start our session by providing you with an outline. Please respond that you received it and then wait for further instructions.
1. Claim Submission
Accurate claim submission is vital in medical billing. It’s the first vital service that medical billing companies offer healthcare providers. It’s not just about sending bills to insurance companies; it’s about sending them correctly.
Accurate claim submission ensures that your claims are processed swiftly, and your revenue flows inconsistently. Medical billing companies employ skilled professionals who understand the nuances of submitting claims, coding, documentation, and adhering to insurance guidelines.
Entrusting this task to experts will let you reduce the risk of claim denials, which often occur due to errors in the submission process. Denied claims can result in delayed payments, increased administrative work, and revenue loss. On the other hand, accurate claim submission will help you avoid these pitfalls and focus on patient care.
2. Coding And Documentation
The second crucial service offered by medical billing companies is coding and documentation. Accurate coding ensures that the medical services you provide are properly represented on insurance claims.
Medical billing companies have certified coders who understand the latest coding guidelines and regulations. They’ll keenly review your documentation to ensure that the codes accurately reflect the services rendered. This attention to detail is essential for two reasons: claim acceptance and revenue optimization.
When your claims include the correct codes, insurance companies are more likely to accept them without delay. Incorrect codes can lead to claim denials or down coding, which can reduce your reimbursement.
3. Insurance Verification

This service might not be the most glamorous task, but it’s undeniably crucial. Why? Because it prevents surprises down the road. Verifying patient insurance details upfront can save you from headaches caused by denied claims and patient disputes.
Medical billing companies take this responsibility seriously. They verify each patient’s insurance coverage to determine if it’s active and valid for the services to be provided. Doing this minimizes the risk of claim denials due to ineligible or expired insurance.
Furthermore, insurance verification helps in estimating patient responsibility accurately. Patients are more likely to understand and pay their bills when they have a clear understanding of their financial obligations. Thus, this service not only streamlines the revenue cycle but also contributes to patient satisfaction.
4. Patient Billing And Collections
Patient billing can be a daunting task for healthcare providers. Managing statements, following up on unpaid bills, and handling patient collections can be time-consuming and uncomfortable.
Medical billing companies handle patient billing and collections with professionalism and sensitivity. They send out clear and concise statements to patients, making it easier for them to understand their obligations. Also, they provide a point of contact for patients to address any billing questions or concerns.
Efficient patient billing and collections can improve your cash flow and enhance patient satisfaction. Patients are also likely to appreciate transparency in billing. Fortunately, outsourcing this service can offer a smoother financial experience for your patients.
5. Payment Posting And Reconciliation

These are vital cogs in the medical billing machinery. Accurate recording of payments and reconciliation with claims will make sure that your practice’s financial records remain pristine.
Medical billing companies have automated systems and dedicated staff to handle this task. They match incoming payments with the corresponding claims, ensuring that every payment is accounted for. This approach safeguards against errors and discrepancies in financial records.
The importance of accurate payment posting extends beyond mere bookkeeping. It lets you receive the correct amount for your services and addresses any discrepancies or underpayments. Moreover, it enhances financial transparency and integrity, which can be invaluable during audits
6. Denial Management
Claim denials are a persistent challenge in healthcare billing, often stemming from errors or miscommunication. They can occur for various reasons, including incomplete information, coding errors, or missing documentation.
Medical billing companies tackle this issue head-on to minimize revenue loss and improve cash flow. If you hire them, they’ll conduct thorough reviews to identify and address your problems.
When a claim is denied, timely and effective action is crucial. Billing companies have experienced professionals who can navigate the appeals process, overturn denials, and increase your organization’s revenue. With a professional by your side in place, you’ll have fewer claim denials and experience faster resolution when denials occur. This can directly contribute to improved cash flow and overall financial stability.
7. Reporting And Analytics
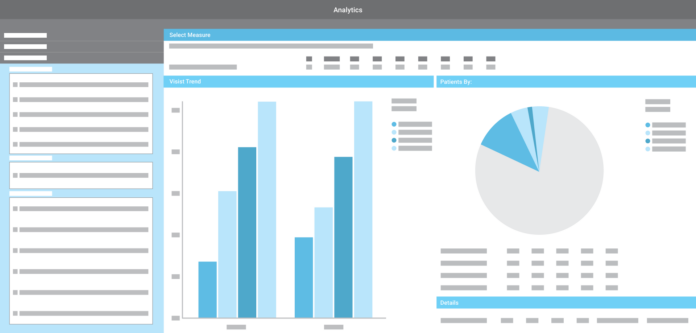
In the current data-driven world, healthcare practices can’t afford to overlook the power of reporting and analytics. This duo offers a holistic view of your practice’s financial performance, revealing trends, opportunities, and areas for improvement.
Billing companies can provide valuable insights to enhance your decision-making process. Using advanced software, they generate customized reports, interpret the data, highlight key performance indicators, and suggest strategies for improvement.
Armed with data-driven insights, healthcare providers can make informed decisions to optimize their practice operations. Whether it’s adjusting pricing strategies or refining workflows, these insights can pave the way for enhanced efficiency and profitability
The Bottom Line
Medical billing companies offer an array of essential services that can transform the financial health and operational efficiency of healthcare practices like yours. From accurate claim submission to data-driven insights, these services not only save time and resources but also contribute to improved patient satisfaction and practice growth.
Consider the tremendous benefits of outsourcing your medical billing needs to professionals who specialize in this field. Working with professionals will let you redirect your focus to what matters most. You’ll also safeguard your medical billing business income and position your hospital for a more prosperous future.







