The state of your metabolic health is largely reflected in your blood sugar levels. Simply put, glucose levels are a key indicator that deserves your attention. Glucose provides the fuel your cells need to function, so controlling it is a top health priority. The body masterfully juggles blood sugar levels, expertly balancing the counteracting forces of insulin and glucagon to maintain harmony.
Insulin, produced by the pancreas, facilitates the uptake of glucose into cells, while glucagon works to release glucose stored in the liver when blood sugar levels drop. Step out of balance and your blood sugar levels can careen wildly, plunging you into the dangerous territory of hypoglycemia or hyperglycemia – conditions that demand attention and care to manage effectively.
Chronic high blood sugar levels are often associated with insulin resistance, a condition where the body’s cells become less responsive to insulin. From local communities to international hubs, type 2 diabetes – with its elevated blood sugar and far-reaching implications – weighs heavily on millions of people’s daily lives. High blood sugar levels set off a domino effect, putting your heart, nerves, kidneys, and eyes in harm’s way.
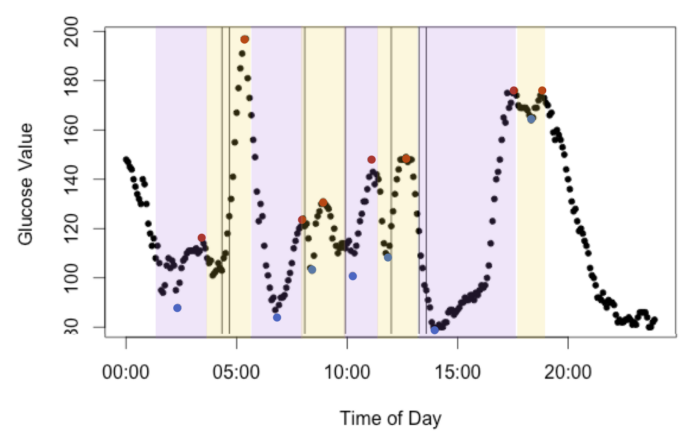
Unchecked, they can trigger a range of problems, from cardiovascular disease to vision loss. Blood sugar levels don’t stay stagnant – they’re constantly shifting based on the food you fuel your body with, your activity level, stress, and sleep patterns, making it vital to stay on top of these factors for optimal health. Say goodbye to the threat of chronic health issues by simply staying on top of your blood sugar levels – it’s a habit that can pay off in a big way.
Intermittent Fasting: A Simple Solution for Balanced Blood Sugar

Fasting in fits and starts – intermittent fasting, for short – has captured the attention of dieters and health enthusiasts alike. One of its standout benefits? Blood sugar control. It’s a simple yet powerful concept: eat, then fast, and repeat – with each cycle varying in length to keep your body on its toes.
By imposed fasting periods, our bodies can reboot and fine-tune their internal mechanics – one astonishing byproduct being tighter blood sugar control that can revolutionize metabolic health. Take charge of your body’s response to sugar with IF, which helps mend the communication breakdown between cells and insulin, releasing energy flows. Anyone facing a high risk of type 2 diabetes or who’s already walking that daily tightrope can really reap the rewards of this.
Imagine experiencing steady energy and blood sugar levels without the typical dips and spikes – that’s exactly what intermittent fasting can deliver. By limiting the time frame in which food is consumed, individuals may experience fewer spikes and crashes in their blood sugar levels.
The result of stabilization? You’ll have more zip in your step and less temptation to reach for sugary snacks, which can throw your blood sugar out of whack. Fasting intermittently appears to give the body a leg up on fat metabolism, resulting in a healthier metabolic profile. Fasting in intervals can have a dual benefit: it helps people shed pounds and keeps their blood sugar levels in check. For more tips and resources on intermittent fasting and blood sugar management, explore https://www.drberg.com/blog.
Intermittent Fasting: A Path to Better Insulin Control
Interlude of life often reveals an unlikely friend in metabolism maintenance, prompting the question: what about weaning dietary vigilance and slathering hormones up to balance? Intermittent fasting slips quietly into this scene, altering how we perceive energy utilization. During fasting periods, insulin levels naturally decrease as the body shifts from using glucose as its primary energy source to utilizing stored fat.
This reduction in insulin not only allows for fat burning but also gives the pancreas a much-needed break from constant stimulation. This gradual shift can bring a welcome change: your body begins to respond better to insulin and is able to manage blood sugar with less of it. Intermittent fasting has been put to the test, and the results are promising: it leads to significant decreases in fasting insulin levels.
For instance, a study published in the journal “Cell Metabolism” found that participants who engaged in intermittent fasting experienced a marked decrease in insulin levels compared to those who followed a traditional eating pattern. Insulin levels don’t have to be the bad guy. When they’re lower, weight gain and fat storage – those unwelcome friends – are less likely to show up. What is the upside of insulin leveling out during fasting? It opens the door to efficient weight loss, impressive body recomposition, and outstanding blood sugar regulation – all at the same time.
The Role of Intermittent Fasting in Improving Insulin Sensitivity
Insulin sensitivity refers to how responsive the body’s cells are to insulin’s effects. Higher insulin sensitivity means that cells can effectively take up glucose from the bloodstream with less insulin required. Insulin sensitivity gets a significant lift when you incorporate intermittent fasting into your lifestyle, thanks to a multi-pronged biochemical response. One key factor is the reduction in overall caloric intake that often accompanies intermittent fasting.
When individuals eat fewer calories over time, it can lead to weight loss and a decrease in visceral fat—fat stored around internal organs—which is closely linked to insulin resistance. When you adopt intermittent fasting, your cells get a fresh chance to heal and regenerate while inflammation subsides, setting the stage for more efficient insulin function. During fasting periods, the body initiates autophagy, a process where cells remove damaged components and regenerate themselves.
When cells get a rejuvenation boost, they start cranking out energy and responding to insulin with ease. By simplifying their eating habits through intermittent fasting, people are already reaping the rewards: after just a short while, they’re experiencing marked enhancements in insulin sensitivity. You’d be hard-pressed to find a dieting approach that rivals intermittent fasting when it comes to delivery – it simultaneously tackles weight management and metabolic function, yielding impressive results for those who stick to it.
Normalize Blood Sugar Spikes with Intermittent Fasting
Incorporating intermittent fasting into a blood sugar management plan requires careful consideration and planning. One effective approach is to start with a simple 16/8 method, where individuals fast for 16 hours each day and eat during an 8-hour window. This can be achieved by skipping breakfast and having lunch as the first meal of the day. Think of your eating window as a chance to refuel with whole, nutritious foods.
Opt for lean proteins like chicken, fish, and tofu paired with fiber-rich veggies and whole grains. With stable blood sugar levels, your body gets a shot of stability, and as a bonus, essential nutrients kick in to supercharge your overall health. Don’t let dehydration sabotage your fasting goals; make hydration a top priority during those zero-calorie hours. Drinking water, herbal teas, or black coffee can help curb hunger pangs and keep individuals feeling full without adding calories.
Additionally, it’s beneficial to listen to one’s body; if feelings of extreme hunger or fatigue arise during fasting periods, it may be necessary to adjust the fasting schedule or consult with a healthcare professional for personalized guidance. What if you could pinpoint which foods propelled your blood sugar levels in the right direction – and which ones derailed them? Regular monitoring provides this precise feedback, allowing you to adapt your eating habits and intermittent fasting strategy with confidence for reviewing fasting guidelines provided by the U.S. Department of Health & Human Services.
Risks and Considerations of Intermittent Fasting for Blood Sugar Control

While intermittent fasting offers numerous benefits for managing blood sugar levels, it is not without potential risks and considerations. Individuals with certain medical conditions—such as diabetes—should approach intermittent fasting with caution. For those on medication that lowers blood sugar, fasting could lead to hypoglycemia if not carefully monitored.
To avoid any potential risks, individuals looking too fast should work hand-in-hand with their healthcare providers to develop a fasting plan that’s sensitive to their distinct health concerns and prescription medications. Moreover, intermittent fasting may not be suitable for everyone. People with a history of eating disorders or those who struggle with disordered eating patterns may find that restrictive eating windows exacerbate unhealthy behaviors or thoughts around food.
Additionally, pregnant or breastfeeding women should avoid intermittent fasting unless advised otherwise by a healthcare professional due to increased nutritional needs during these critical periods. Considering intermittent fasting for blood sugar control? First, carefully weigh your personal health circumstances – and don’t hesitate to consult a healthcare pro if needed – to sidestep potential risks and maximize benefits.







